As we head into the holiday season, Cancer Research Catalyst has tantalizing teasers in the form of science stocking stuffers straight from our November edition of Editors’ Picks. This month, the editors of the 10 American Association for Cancer Research (AACR) journals selected studies covering the immune-boosting benefits of dietary restriction, novel therapies like nanovaccines and p53-targeting peptides, and health disparities in specific communities, including chronic conditions in LGBTQ+ cancer survivors and cervical cancer in Native American women.
Read the abstracts below or follow the links to the full articles, which are freely available for a limited time.
JOURNAL: BLOOD CANCER DISCOVERY
Multiple Myeloma Risk and Outcomes Are Associated with Pathogenic Germline Variants in DNA Repair Genes
First-degree relatives of patients with multiple myeloma are at increased risk for the disease, but the contribution of pathogenic germline variants (PGV) in hereditary cancer genes to multiple myeloma risk and outcomes is not well characterized. To address this, we analyzed germline exomes in two independent cohorts of 895 and 786 patients with multiple myeloma. PGVs were identified in 8.6% of the Discovery cohort and 11.5% of the Replication cohort, with a notable presence of high- or moderate-penetrance PGVs (associated with autosomal dominant cancer predisposition) in DNA repair genes (3.6% and 4.1%, respectively). PGVs in BRCA1 (OR = 3.9, FDR < 0.01) and BRCA2 (OR = 7.0, FDR < 0.001) were significantly enriched in patients with multiple myeloma when compared with 134,187 healthy controls. Five of the eight BRCA2 PGV carriers exhibited tumor-specific copy number loss in BRCA2, suggesting somatic loss of heterozygosity. PGVs associated with autosomal dominant cancer predisposition were associated with younger age at diagnosis, personal or familial cancer history, and longer progression-free survival after upfront high-dose melphalan and autologous stem-cell transplantation (P < 0.01).
Significance: Our findings suggest up to 10% of patients with multiple myeloma may have an unsuspected cancer predisposition syndrome. Given familial implications and favorable outcomes with high-dose melphalan and autologous stem-cell transplantation in high-penetrance PGV carriers, genetic testing should be considered for young or newly diagnosed patients with a personal or family cancer history.
A related commentary was published in the November issue.
JOURNAL: CANCER DISCOVERY
T-cell Responses to Individualized Neoantigen Therapy mRNA-4157 (V940) Alone or in Combination with Pembrolizumab in the Phase 1 KEYNOTE-603 Study
mRNA-4157 (V940) is an individualized neoantigen therapy targeting up to 34 patient-specific tumor neoantigens to induce T-cell responses and potentiate antitumor activity. We report mechanistic insights into the immunogenicity of mRNA-4157 via characterization of T-cell responses to neoantigens from the first-in-human, phase 1, KEYNOTE-603 study (NCT03313778) in patients with resected non–small cell lung cancer (Part A: 1-mg mRNA-4157, n = 4) or resected cutaneous melanoma (Part D: 1-mg mRNA-4157 + 200-mg pembrolizumab, n = 12). Safety, tolerability, and immunogenicity were assessed. All patients experienced ≥1 treatment-emergent adverse event; there were no grade 4/5 adverse events or dose-limiting toxicities. mRNA-4157 alone induced consistent de novo and strengthened preexisting T-cell responses to targeted neoantigens. Following combination therapy, sustained mRNA-4157-induced neoantigen-specific T-cell responses and expansion of cytotoxic CD8 and CD4 T cells were observed. These findings show the potential of a novel mRNA individualized neoantigen therapy approach in oncology.
Significance: The safety and immunogenicity results from this phase 1 study of mRNA-4157 as adjuvant monotherapy or combination therapy with pembrolizumab show generation of de novo and enhancement of existing neoantigen-specific T-cell responses and provide mechanistic proof of concept to support further development of mRNA-4157 for patients with resected solid tumors.
A related commentary was published in the November issue. This issue also had a special collection of articles from Chinese researchers. Learn more about this collection.
JOURNAL: CANCER EPIDEMIOLOGY, BIOMARKRS & PREVENTION
Chronic Health Conditions, Disability, and Physical and Cognitive Limitations among LGBTQ+ Cancer Survivors
Background: Cancer survivors are at high risk for chronic health conditions and physical and cognitive limitations. However, few studies have explored these outcomes among Lesbian, Gay, Bisexual, Transgender, Queer, Plus (LGBTQ+) survivors.
Methods: We used pooled, weighted Behavioral Risk Factor Surveillance System data from 23 states that completed two specific modules at least once from 2020 to 2022. We calculated age-adjusted prevalence for heart disease, asthma, chronic obstructive pulmonary disease, depressive disorders, myocardial infarction, kidney disease, stroke, diabetes, hearing disability, vision disability, cognitive limitations, and difficulty walking, dressing, and running errands in LGBTQ+, lesbian, gay, or bisexual, transgender or gender nonconforming (TGNC), and non-LGBTQ+ cancer survivors. Four multivariable logistic regression models controlling for different factors were run for each outcome.
Results: Of 40,990 cancer survivors, 1,715 were LGBTQ+. LGBTQ+ survivors had significantly higher age-adjusted prevalence of all outcomes. The prevalence of all outcomes was the highest among TGNC survivors, except for depressive disorders and cognitive limitations. LGBTQ+ survivors had higher odds of reporting asthma [adjusted OR (aOR): 1.5; 95% confidence interval (CI), 1.2–1.9], depressive disorders (aOR: 1.9; 95% CI, 1.6–2.4), kidney disease (aOR: 1.5; 95% CI, 1.1–2.1), stroke (aOR: 1.7; 95% CI, 1.3–2.3), diabetes (aOR: 1.3; 95% CI, 1.0–1.6), vision disability (aOR: 1.6; 95% CI, 1.2–2.2), cognitive limitations (aOR: 2.3; 95% CI, 1.8–2.9), difficulty walking (aOR: 1.7; 95% CI, 1.3–2.0), dressing (aOR: 2.0; 95% CI, 1.5–2.7), and running errands (aOR: 1.6; 95% CI, 1.3–2.1). In TGNC models, TGNC cancer survivors had increased odds of most outcomes in comparison to cisgender survivors.
Conclusions: LGBTQ+ cancer survivors have an elevated burden of all chronic health conditions, disabilities, and limitations assessed. TGNC cancer survivors experience even higher burden of the same outcomes.
Impact: Findings highlight substantial disparities regarding the health of LGBTQ+ cancer survivors.
A related commentary was published in the November issue. This study was also covered as part of a blog post on LGBTQ+ cancer survivors.
JOURNAL: CANCER IMMUNOLOGY RESEARCH
A Single-Cell Analysis of the NK-Cell Landscape Reveals That Dietary Restriction Boosts NK-Cell Antitumor Immunity via Eomesodermin
Abnormal metabolism in tumor cells represents a potential target for tumor therapy. In this regard, dietary restriction or its combination with anticancer drugs is of interest as it can impede the growth of tumor cells. In addition to its effects on tumor cells, dietary restriction also plays an extrinsic role in restricting tumor growth by regulating immune cells. NK cells are innate immune cells involved in tumor immunosurveillance. However, it remains uncertain whether dietary restriction can assist NK cells in controlling tumor growth. In this study, we demonstrate that dietary restriction effectively inhibits metastasis of melanoma cells to the lung. Consistent with this, the regression of tumors induced by dietary restriction was minimal in mice lacking NK cells. Single-cell RNA sequencing analysis revealed that dietary restriction enriched a rejuvenated subset of CD27+CD11b+ NK cells. Mechanistically, dietary restriction activated a regulatory network involving the transcription factor Eomesodermin (Eomes), which is essential for NK-cell development. First, dietary restriction promoted the expression of Eomes by optimizing mTORC1 signaling. The upregulation of Eomes revived the subset of functional CD27+CD11b+ NK cells by counteracting the expression of T-bet and downstream Zeb2. Moreover, dietary restriction enhanced the function and chemotaxis of NK cells by increasing the accessibility of Eomes to chromatin, leading to elevated expression of adhesion molecules and chemokines. Consequently, we conclude that dietary restriction therapy enhances tumor immunity through nontumor autonomous mechanisms, including promoting NK-cell tumor immunosurveillance and activation.
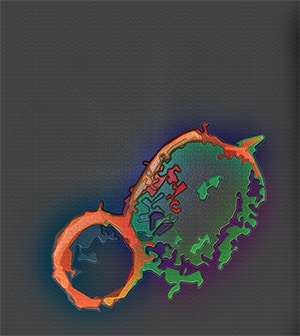
This story was featured on the cover of the November issue.
JOURNAL: CANCER PREVENTION RESEARCH
Viewing Native American Cervical Cancer Disparities through the Lens of the Vaginal Microbiome: A Pilot Study
Vaginal dysbiosis is implicated in persistent human papillomavirus (HPV) infection and cervical cancer. Yet, there is a paucity of data on the vaginal microbiome in Native American communities. Here, we aimed to elucidate the relationships between microbiome, HPV, sociodemographic, and behavioral risk factors to better understand an increased cervical cancer risk in Native American women. In this pilot study, we recruited 31 participants (16 Native American and 15 non-Native women) in Northern Arizona and examined vaginal microbiota composition, HPV status, and immune mediators. We also assessed individuals’ sociodemographic information and physical, mental, sexual, and reproductive health. Overall, microbiota profiles were dominated by common Lactobacillus species (associated with vaginal health) or a mixture of bacterial vaginosis–associated bacteria. Only 44% of Native women exhibited Lactobacillus dominance, compared with 58% of non-Native women. Women with vaginal dysbiosis also had elevated vaginal pH and were more frequently infected with high-risk HPV. Furthermore, we observed associations of multiple people in a household, lower level of education, and high parity with vaginal dysbiosis and abundance of specific bacterial species. Finally, women with dysbiotic microbiota presented with elevated vaginal levels of proinflammatory cytokines. Altogether, these findings indicate an interplay between HPV, vaginal microbiota, and host defense, which may play a role in the cervical cancer disparity among Native American women. Future longitudinal studies are needed to determine the mechanistic role of vaginal microbiota in HPV persistence in the context of social determinants of health toward the long-term goal of reducing health disparities between non-Hispanic White and Native American populations.
Prevention Relevance: Cervical cancer disproportionally affects Native American women. Sociodemographic and behavioral factors might contribute to this disparity via alteration of vaginal microbiota. Here, we show the association between these factors and vaginal dysbiosis and immune activation, which can be implicated in high-risk HPV infection among Native American and other racial/ethnic populations.
This story was featured on the cover of the November issue.
JOURNAL: CANCER RESEARCH
Neuroendocrine Differentiation in Prostate Cancer Requires ASCL1
Most patients with prostate adenocarcinoma develop resistance to therapies targeting the androgen receptor (AR). Consequently, a portion of these patients develop AR-independent neuroendocrine (NE) prostate cancer (NEPC), a rapidly progressing cancer with limited therapies and poor survival outcomes. Current research to understand the progression to NEPC suggests a model of lineage plasticity whereby AR-dependent luminal-like tumors progress toward an AR-independent NEPC state. Genetic analysis of human NEPC identified frequent loss of RB1 and TP53, and the loss of both genes in experimental models mediates the transition to a NE lineage. Transcriptomics studies have shown that lineage transcription factors ASCL1 and NEUROD1 are present in NEPC. In this study, we modeled the progression of prostate adenocarcinoma to NEPC by establishing prostate organoids and subsequently generating subcutaneous allograft tumors from genetically engineered mouse models harboring Cre-induced loss of Rb1 and Trp53 with Myc overexpression (RPM). These tumors were heterogeneous and displayed adenocarcinoma, squamous, and NE features. ASCL1 and NEUROD1 were expressed within NE-defined regions, with ASCL1 being predominant. Genetic loss of Ascl1 in this model did not decrease tumor incidence, growth, or metastasis; however, there was a notable decrease in NE identity and an increase in basal-like identity. This study provides an in vivo model to study progression to NEPC and establishes the requirement for ASCL1 in driving NE differentiation in prostate cancer.
Significance: Modeling lineage transitions in prostate cancer and testing dependencies of lineage transcription factors have therapeutic implications, given the emergence of treatment-resistant, aggressive forms of neuroendocrine prostate cancer.
A related commentary was published in the November 1 issue.
JOURNAL: CANCER RESEARCH
Precise In Situ Delivery of a Photo-Enhanceable Inflammasome-Activating Nanovaccine Activates Anticancer Immunity
A variety of state-of-the-art nanovaccines combined with immunotherapies have recently been developed to treat malignant tumors, showing promising results. However, immunosuppression in the tumor microenvironment (TME) restrains cytotoxic T-cell infiltration and limits the efficacy of immunotherapies in solid tumors. Therefore, tactics for enhancing antigen cross-presentation and reshaping the TME need to be explored to enhance the activity of nanovaccines. Here, we developed photo-enhanceable inflammasome-activating nanovaccines (PIN) to achieve precise in situ delivery of a tumor antigen and a hydrophobic small molecule activating the nucleotide-binding oligomerization domain, leucine-rich repeat, and pyrin domain–containing protein 3 inflammasome (NLRP3) pathway. Near-infrared light irradiation promoted PIN accumulation in tumor sites through photo-triggered charge reversal of the nanocarrier. Systematic PIN administration facilitated intratumoral NLRP3 inflammasome activation and antigen cross-presentation in antigen-presenting cells upon light irradiation at tumor sites. Furthermore, PIN treatment triggered immune responses by promoting the production of proinflammatory cytokines and activating antitumor immunity without significant systematic toxicity. Importantly, the PIN enhanced the efficacy of immune checkpoint blockade and supported the establishment of long-term immune memory in mouse models of melanoma and hepatocellular carcinoma. Collectively, this study reports a safe and efficient photoresponsive system for codelivery of antigens and immune modulators into tumor tissues, with promising therapeutic potential.
Significance: The development of a photoresponsive nanovaccine with spatiotemporal controllability enables robust tumor microenvironment modulation and enhances the efficacy of immune checkpoint blockade, providing an effective immunotherapeutic strategy for cancer treatment.
A related commentary was published in the November 15 issue.
JOURNAL: CLINICAL CANCER RESEARCH
A Phase II Study of Atezolizumab, Pertuzumab, and High-Dose Trastuzumab for Central Nervous System Metastases in Patients with HER2-Positive Breast Cancer
Purpose: Patients with HER2-positive breast cancer brain metastases have few effective systemic therapy options. In a prior study, pertuzumab with high-dose trastuzumab demonstrated a high clinical benefit rate (CBR) in the central nervous system (CNS) in patients with brain metastases. The current trial evaluated whether the addition of atezolizumab to this regimen would produce further improvements in CNS response.
Patients and Methods: This was a single-arm, multicenter, phase II trial of atezolizumab, pertuzumab, and high-dose trastuzumab for patients with HER2-positive breast cancer brain metastases. Participants received atezolizumab 1,200 mg i.v. every 3 weeks, pertuzumab (loading dosage 840 mg i.v., then 420 mg i.v. every 3 weeks), and high-dose trastuzumab (6 mg/kg i.v. weekly for 24 weeks, then 6 mg/kg i.v. every 3 weeks). The primary endpoint was CNS overall response rate per Response Assessment in Neuro-Oncology Brain Metastases criteria. Key secondary endpoints included CBR, overall survival, and safety and tolerability of the combination.
Results: Among 19 enrolled participants, two had a confirmed intracranial partial response for a CNS overall response rate of 10.5% (90% confidence interval, 1.9%–29.6%). The study did not meet the prespecified efficacy threshold and was terminated early. The CBR was 42.1% at 18 weeks and 31.6% at 24 weeks. Seven patients (36.8%) required a dose delay or hold, and the most frequent any-grade adverse events were diarrhea (26.3%) and fatigue (26.3%).
Conclusions: The addition of atezolizumab to pertuzumab plus high-dose trastuzumab does not result in improved CNS responses in patients with HER2-positive breast cancer brain metastases.
JOURNAL: CLINICAL CANCER RESEARCH
A Phase I First-in-Human Study of ABBV-011, a Seizure-Related Homolog Protein 6–Targeting Antibody–Drug Conjugate, in Patients with Small Cell Lung Cancer
Purpose: Seizure-related homolog protein 6 (SEZ6) is a novel target expressed in small cell lung cancer (SCLC). ABBV-011, a SEZ6-targeted antibody conjugated to calicheamicin, was evaluated in a phase I study (NCT03639194) in patients with relapsed/refractory SCLC. We report initial outcomes of ABBV-011 monotherapy.
Patients and Methods: ABBV-011 was administered intravenously once every 3 weeks during dose escalation (0.3–2 mg/kg) and expansion. Patients with SEZ6-positive tumors (≥25% of tumor cells with ≥1+ staining intensity by IHC) were preselected for expansion. Safety, tolerability, antitumor activity, and pharmacokinetics were evaluated.
Results: As of August 2022, 99 patients received ABBV-011 monotherapy [dose escalation, n = 36; Japanese dose evaluation, n = 3; dose expansion, n = 60 (1 mg/kg, n = 40)]; the median age was 63 years (range, 41–79 years). Also, 32%, 41%, and 26% of patients received 1, 2, and ≥3 prior therapies, respectively. The maximum tolerated dose was not reached through 2.0 mg/kg. The most common treatment-emergent adverse events were fatigue (50%), nausea (42%), and thrombocytopenia (41%). The most common hepatic treatment-emergent adverse events were increased aspartate aminotransferase (22%), increased γ-glutamyltransferase (21%), and hyperbilirubinemia (17%); two patients experienced veno-occlusive liver disease. The objective response rate was 19% (19/98). In the 1-mg/kg dose-expansion cohort (n = 40), the objective response rate was 25%; the median response duration was 4.2 months (95% confidence interval, 2.6–6.7); and the median progression-free survival was 3.5 months (95% confidence interval, 1.5–4.2).
Conclusions: ABBV-011 1.0 mg/kg every 3 weeks monotherapy was well tolerated and demonstrated encouraging antitumor activity in heavily pretreated patients with relapsed/refractory SCLC. SEZ6 is a promising novel SCLC target and warrants further investigation.
JOURNAL: MOLECULAR CANCER RESEARCH
GRAIL1 Stabilizes Misfolded Mutant p53 through a Ubiquitin Ligase-Independent, Chaperone Regulatory Function

Frequent (>70%) TP53 mutations often promote its protein stabilization, driving esophageal adenocarcinoma (EAC) development linked to poor survival and therapy resistance. We previously reported that during Barrett’s esophagus progression to EAC, an isoform switch occurs in the E3 ubiquitin ligase RNF128 (aka GRAIL—gene related to anergy in lymphocytes), enriching isoform 1 (hereby GRAIL1) and stabilizing the mutant p53 protein. Consequently, GRAIL1 knockdown degrades mutant p53. But, how GRAIL1 stabilizes the mutant p53 protein remains unclear. In search for a mechanism, here, we performed biochemical and cell biology studies to identify that GRAIL has a binding domain (315-PMCKCDILKA-325) for heat shock protein 40/DNAJ. This interaction can influence DNAJ chaperone activity to modulate misfolded mutant p53 stability. As predicted, either the overexpression of a GRAIL fragment (Frag-J) encompassing the DNAJ binding domain or a cell-permeable peptide (Pep-J) encoding the above 10 amino acids can bind and inhibit DNAJ-Hsp70 co-chaperone activity, thus degrading misfolded mutant p53. Consequently, either Frag-J or Pep-J can reduce the survival of mutant p53 containing dysplastic Barrett’s esophagus and EAC cells and inhibit the growth of patient-derived organoids of dysplastic Barrett’s esophagus in 3D cultures. The misfolded mutant p53 targeting and growth inhibitory effects of Pep-J are comparable with simvastatin, a cholesterol-lowering drug that can degrade misfolded mutant p53 also via inhibiting DNAJA1, although by a distinct mechanism.
Implications: We identified a novel ubiquitin ligase-independent, chaperone-regulating domain in GRAIL and further synthesized a first-in-class novel misfolded mutant p53 degrading peptide having future translational potential.
This story was featured on the cover of the November issue.
JOURNAL: MOLECULAR CANCER THERAPEUTICS
Dual A2A/A2B Adenosine Receptor Antagonist M1069 Counteracts Immunosuppressive Mechanisms of Adenosine and Reduces Tumor Growth In Vivo
While A2A adenosine receptor (AR) was considered as a major contributor to adenosine-mediated immunosuppression, A2B, having the lowest affinity to adenosine, has also emerged as a potential contributor to tumor promotion. Therefore, in adenosine-rich tumor microenvironment (TME), where A2B could be complementary and/or compensatory to A2A, simultaneous targeting of A2A and A2B ARs can provide higher potential for cancer immunotherapy. We developed M1069—a highly selective dual antagonist of the A2A and A2B AR. In assays with primary human and murine immune cells, M1069 rescued IL2 production from T cells (A2A dependent) and inhibited VEGF production by myeloid cells (A2B dependent) in adenosine-high settings. M1069 also demonstrated superior suppression of the secretion of protumorigenic cytokines CXCL1, CXCL5, and rescue of IL12 secretion from adenosine-differentiated dendritic cells compared to an A2A-selective antagonist (A2Ai). In a one-way mixed lymphocyte reaction (MLR) assay, adenosine-differentiated human and murine dendritic cells treated with M1069 demonstrated superior T-cell stimulatory activity compared to dendritic cells differentiated in presence of A2Ai. In vivo, M1069 decreased tumor growth as a monotherapy and enhanced antitumor activity of bintrafusp alfa (BA) or cisplatin in syngeneic adenosinehi/CD73hi 4T1 breast tumor model, but not in the CD73 knockout 4T1 tumor model or in adenosinelow/CD73low MC38 murine colon carcinoma model. In summary, our dual A2A/A2B AR antagonist M1069 may counteract immune-suppressive mechanisms of high concentrations of adenosine in vitro and in vivo and enhance the antitumor activity of other agents, including BA and cisplatin.
This story was featured on the cover of the November issue.
JOURNAL: CANCER RESEARCH COMMUNICATIONS
Health Disparities among Patients with Cancer Who Received Molecular Testing for Biomarker-Directed Therapy
Health disparities present a barrier to successful oncology treatment. The potential for precision oncology to reduce health disparities has not previously been analyzed. We performed a retrospective analysis of 12,627 patients from six major cancer centers whose tumors underwent molecular testing at Caris Life Sciences between 2010 and 2020. Kaplan–Meier and Cox regression were used to describe and analyze overall survival. The molecular and demographic features of the cohort were analyzed by χ2 and ANOVA tests. Black patients composed 25% of the cohort and White patients 63%. Among this molecularly-tested cohort, there were minimal outcome differences based on race, geographic location, or poverty level. When analyzing the interaction of age, race, and sex, racial-based disparities were noted primarily for young non-White women in the study cohort but were more pronounced for men and women of all ages in the broader patient population within the Surveillance, Epidemiology, and End Results database. Mutations in five genes—APC, EGFR, STK11, TP53, and KRAS—were found to affect overall survival among our cohort, and their prevalence varied by race in specific tumor types. Real-world outcomes data in mutation-defined cohorts also provided additional context to previously reported therapeutic response trends. Our study shows that patients who undergo molecular testing display reduced racial health disparities compared with the general population, whereas persistent racial disparities are influenced by age and sex. Genomic-driven racial disparities should be examined at a tumor lineage-specific level. Increased access to molecular testing for all eligible patients may play a role in improving health equity.
Significance: This study is the largest of its kind to analyze health disparities and genomic features among a diverse multiinstitutional cohort of patients who underwent molecular testing. Continuing to increase awareness of and access to molecular testing approaches may help to reduce cancer health disparities and improve outcomes for all patients.


