To help our readers keep track of the cancer therapies approved by the U.S. Food and Drug Administration (FDA), understand their impact for patients, and put them in context of the current therapeutic landscape, Cancer Research Catalyst provides a quarterly review of the latest approvals from the FDA.
The second quarter of 2024 featured big advances for immunotherapy, with the first bispecific T-cell engager approved for a solid cancer type, an early-stage indication for another bispecific T-cell engager, a new class of immunotherapy for bladder cancer, two new indications for chimeric antigen receptor (CAR) T-cell therapy, and new indications for immune checkpoint inhibitors.
This quarter also gave us new tissue-agnostic approvals, the first direct inhibitor of telomerase, several new approvals for pediatric cancer, and new indications for various targeted therapies.
Keep reading to learn about these approvals and how they fit into the treatment landscape. For more information, including the clinical data that led to each approval, check out our FDA approvals page.
First Bispecific T-cell Engager for Solid Cancer
Bispecific T-cell engagers are a type of immunotherapy that help T cells find cancer cells so they can attack and kill them. They work by simultaneously binding proteins on both cancer cells and T cells, thereby bringing the two cell types together. These therapeutics have been approved for many blood cancers, but they have been less successful at treating solid cancer types, in large part because the cancer cells that make up solid tumors tend to have fewer cancer-specific proteins on their surfaces to target.
Despite this challenge, researchers were able to develop a bispecific T-cell engager that successfully treated patients with a type of lung cancer, leading to the first approval for this class of therapeutic for a solid cancer type, which was issued this quarter.
- Tarlatamab (Imdelltra) received accelerated approval to treat patients with extensive-stage small cell lung cancer (ES-SCLC) that progressed during or after prior chemotherapy. ES-SCLC is an aggressive form of lung cancer prone to disease progression and associated with a high death rate.
This is the first FDA approval for tarlatamab, which simultaneously binds the delta-like ligand 3 (DLL3) protein on cancer cells and the CD3 protein on T cells. DLL3 is normally found inside of cells, but in cancer cells, it is often expressed on the cell surface—making it an ideal target for bispecific T-cell engager therapy.
Bispecific T-cell Engagers Approved for Additional Patients with Blood Cancer
Another first for bispecific T-cell engager therapy this quarter was its approval as an early treatment for certain leukemias. Prior to this, these therapies were only approved for cancers that persisted, progressed, or relapsed after earlier lines of treatments.
- Blinatumomab (Blincyto) was approved to treat certain adult and pediatric patients with B-cell acute lymphoblastic leukemia (B-ALL) as part of consolidation therapy, a stage of treatment intended to kill any remaining cancer cells in the patient’s body. The treatment is intended for patients whose B-ALL expresses CD19 but does not harbor a mutation known as the Philadelphia chromosome. Unlike prior approvals, this approval makes blinatumomab available to patients whether or not they have confirmed residual disease (i.e., persisting cancer cells) and before their disease has relapsed.
Blinatumomab binds to CD3 on T cells and CD19 on leukemia cells to bring the cells in proximity to each other. This therapeutic was previously approved for patients with CD19-positive B-ALL who are in remission but test positive for residual disease, as well as for patients whose B-ALL relapsed or did not respond to prior treatment.
In addition, another bispecific T-cell engager was approved for patients with follicular lymphoma that relapsed or was refractory to prior lines of treatment.
- Epcoritamab (Epkinly) was granted accelerated approval for adult patients with relapsed or refractory follicular lymphoma who have received at least two prior lines of systemic therapy. Epcoritamab is the second bispecific T-cell engager approved for this patient population; it was previously approved to treat certain other relapsed or refractory B-cell cancers.
First-in-class Therapeutics Make Their Debut
This quarter, the FDA approved two first-in-class drugs that use novel mechanisms to treat cancer: a new type of immunotherapy for bladder cancer and a new type of targeted therapy for blood cancer.
- Nogapendekin alfa inbakicept-pmln (Anktiva) in combination with Bacillus Calmette-Guérin (BCG) was approved to treat certain patients with non-muscle invasive bladder cancer (NMIBC) that has not responded to BCG alone. Nogapendekin alfa inbakicept-pmln works by activating the IL-15 receptor on the surface of some immune cells, which prompts immune cells to proliferate and boosts their activation, so they are better able to fight cancer. This is the first approval for nogapendekin alfa inbakicept-pmln, and the drug is the first IL-15 receptor agonist to be approved by the FDA.
- Imetelstat (Rytelo) was approved to treat certain myelodysplastic syndromes (rare blood cancers) that are unresponsive to or ineligible for medications that stimulate the production of blood cells. Imetelstat inhibits the activity of telomerase, a protein that promotes cancer by elongating DNA ends known as telomeres. This allows cancer cells to keep proliferating beyond what is normal for healthy cells. Imetelstat is the first direct inhibitor of telomerase to receive FDA approval.
Antibody-drug Conjugates Extend Their Reach
Targeted therapies called antibody-drug conjugates use antibody-guided delivery of toxic drugs to cancer cells, while leaving most healthy cells alone. This quarter, the FDA issued approvals for two antibody-drug conjugates.
- Fam-trastuzumab deruxtecan-nxki (Enhertu), also known as T-DXd, was granted a tissue-agnostic accelerated approval for patients with previously treated, unresectable or metastatic HER2-positive solid tumors. T-DXd targets cells that express HER2, which is found at high levels in many breast and gastric cancers and, less frequently, in cancers arising in other tissues. T-DXd was previously approved for certain breast, lung, and gastric cancers.
- The 2021 accelerated approval of tisotumab vedotin-tftv (Tivdak) for patients with recurrent or metastatic cervical cancer after progression on prior chemotherapy was converted to a full approval this quarter. Tisotumab vedotin-tftv targets a protein called tissue factor that is often highly expressed on the surface of cervical cancer cells.
New Indications for Additional Targeted Therapies
In addition to the targeted therapies already discussed, several others received new indications this quarter, including multiple for pediatric patients. These therapies are designed to selectively attack tumors by targeting proteins or alterations often found in cancer cells.
- Selpercatinib (Retevmo) was approved for adults and children aged 2 years or older with certain advanced RET-mutated thyroid cancers. It also received accelerated approval this quarter for pediatric patients 2 years and older with certain locally advanced or metastatic RET-mutated solid tumors, regardless of where they originated. Selpercatinib inhibits mutant forms of the RET tyrosine kinase, a protein that is commonly mutated in several cancer types and can cause tumors to grow faster. Selpercatinib previously received accelerated approval for the same thyroid cancer indications in patients 12 and older in 2020 and for the same solid tumor indication in adults in 2022.
- Tovorafenib (Ojemda) was approved for patients 6 months or older with relapsed or refractory low-grade glioma (a type of brain cancer) that harbors certain BRAF mutations. Tovorafenib inhibits several kinases in the RAF family, including BRAF. When mutated, these kinases can promote uncontrolled cell proliferation and cancer growth. Unlike many other drugs, tovorafenib can cross the blood-brain barrier, allowing it to access cancer cells in the brain. This is the first FDA approval for tovorafenib, which is the first systemic therapy approved for BRAF-mutated low-grade glioma in children.
- Lutetium Lu 177 dotatate (Lutathera) was approved to treat children aged 12 or older with gastroenteropancreatic neuroendocrine tumors (GEP-NETs) that express the somatostatin receptor (SSTR). Lutetium Lu 177 dotatate is a radioactive drug that targets SSTR, a protein highly expressed on the surface of GEP-NET cells. Upon binding to SSTR, lutetium Lu 177 dotatate enters the cell, and the radiation ultimately kills the cell. This drug was previously approved to treat adult patients with SSTR-positive GEP-NETs.
- Repotrectinib (Augtyro) was approved for adult and pediatric patients aged 12 years or older with solid tumors that are locally advanced, metastatic, or ineligible for surgical removal; have progressed after prior treatment; and harbor NTRK gene fusions. In some cancers, a portion of the NTRK gene fuses to another gene, producing a chimeric protein that promotes cancer growth. Repotrectinib inhibits NTRK and other kinases and was previously approved to treat adults with ROS1-positive lung cancers. Because of its unique chemical design, it might be effective against tumors that are resistant to other available NTRK inhibitors.
- Alectinib (Alecensa) was approved for the postsurgical treatment of adults with non-small cell lung cancer (NSCLC) that either overexpresses or has a mutation in the ALK protein. Alectinib inhibits the activity of ALK, a protein that, when mutated, drives tumor growth. Alectinib was previously approved for metastatic NSCLC, and the approval this quarter expanded the use of alectinib to include NSCLC that can be surgically removed.
- Adagrasib (Krazati) in combination with cetuximab (Erbitux) received accelerated approval to treat KRASG12C-mutated locally advanced or metastatic colorectal cancers in adult patients who have received prior chemotherapy. Adagrasib inhibits the activity of the KRASG12C mutant protein that is found in approximately 4% of all colorectal cancers; cetuximab blocks the activity of the epidermal growth factor receptor (EGFR), which, when overexpressed, can help tumors resist the effects of KRAS inhibition. Researchers, therefore, reasoned that inhibiting both KRAS and EGFR might help prevent treatment resistance.
The approval was based on results from the KRYSTAL-1 clinical trial, which were presented at the American Association for Cancer Research (AACR) Annual Meeting 2024 and simultaneously published in the AACR journal Cancer Discovery. This is the first colorectal cancer indication for any KRAS inhibitor. Adagrasib and another KRAS inhibitor, sotorasib (Lumakras), were previously approved for certain lung cancers.
CAR T-cell Therapy for Additional B-cell Cancers
CAR T-cell therapy is a form of immunotherapy in which a patient’s T cells are removed, genetically engineered to recognize a protein on the surface of cancer cells, and infused back into the patient to find and attack cancer cells. Lisocabtagene maraleucel (Breyanzi) is a CAR T-cell therapy that works by targeting the CD19 protein that is highly expressed by malignant B cells. It was previously approved to treat large B-cell lymphoma, chronic lymphocytic leukemia, and small lymphocytic leukemia. This quarter, it was approved for two more B-cell cancers.
- Lisocabtagene maraleucel received accelerated approval to treat patients with relapsed or refractory follicular lymphoma who have already received at least two lines of systemic therapy.
- Lisocabtagene maraleucel was also approved for patients with relapsed or refractory mantle cell lymphoma who previously received two or more lines of systemic therapy, including an inhibitor of Bruton’s tyrosine kinase.
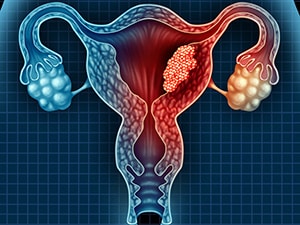
Immune Checkpoint Inhibitors for Endometrial Cancer
Many cancer cells escape the immune response by inactivating T cells, but immunotherapy drugs called immune checkpoint inhibitors can help keep T cells active so they can attack cancer.
Immune checkpoint inhibitors are approved for several indications, and two more were added to the list this quarter—both for advanced or recurrent cases of endometrial cancer.
- Durvalumab (Imfinzi) plus chemotherapy, followed by durvalumab alone, was approved for patients with advanced or recurrent endometrial cancers that have defects in mismatch repair, a type of DNA repair mechanism. Durvalumab binds the PD-L1 protein on cancer and other cells to prevent it from engaging with the PD-1 protein on T cells and turning them “off.” Cancer cells with defective mismatch repair tend to have higher levels of PD-L1. This is durvalumab’s fourth FDA approval and its first for endometrial cancer.
- Pembrolizumab (Keytruda) plus chemotherapy, followed by pembrolizumab alone, was approved for patients with advanced or recurrent endometrial cancers. Pembrolizumab works by binding PD-1 on T cells, thereby preventing PD-L1 on cancer and other cells from engaging with PD-1 and inactivating T cells. Among several other indications, pembrolizumab is also approved in combination with targeted therapy for patients with progressive, mismatch repair-proficient endometrial cancer and as a single-agent for patients with progressive, mismatch repair-deficient endometrial cancer.


