Limited access to cancer care can drive massive disparities in outcomes, causing further harm to already vulnerable populations.
According to the recently published 2024 AACR Cancer Disparities Progress Report, U.S. counties with persistent poverty (20% or more of residents living below the federal poverty level over a 30-year period) had 7.1% more cancer deaths than counties without persistent poverty. Individuals living outside of metropolitan areas were also 19% more likely to die of melanoma, 39% more likely to die of cervical cancer, and 38% more likely to be diagnosed with and die from lung cancer than those living in urban or metropolitan areas.
The issue certainly isn’t unique to the United States. For instance, the cancer mortality-to-incidence ratio in Africa is 39% higher than in North America, with new cancer cases and deaths expected to double by 2040.
At the AACR Annual Meeting 2024, held in San Diego April 5-10, many experts argued that closing the gap will take a global effort, including international collaborations and novel technologies to expand cancer care in under-resourced settings. Here are a handful of the new approaches, initiatives, and implementation strategies discussed at the meeting.
Advanced Drug Screening in South Africa
When cancers develop resistance to standard-of-care therapies, treatment options often become limited, and it can be difficult to decide how to proceed. Researchers around the world are working to develop ex vivo drug screening assays whereby a patient’s tumor tissue is exposed to a panel of drugs in a lab to see which ones might work best.
However, such personalized screening assays are costly and therefore difficult to implement in under-resourced settings. A new screening platform developed in South Africa may be more accessible to African researchers looking to implement these screens in their clinics.
“Ex vivo screening is cost intensive,” said Mutsa Takundwa, PhD, a senior researcher at the Council for Scientific and Industrial Research in South Africa and a 2024 AACR Global Scholar-in-Training Awardee. “This study demonstrates we can do it in an African setting.”
Takundwa and colleagues have developed both cell growth assays and wound healing assays, which measure drugs’ effect on cell migration. They have so far screened 80 samples from patients with leukemia, multiple myeloma, ovarian cancer, or uterine cancer, with an average turnaround time of 14 days, and have identified sensitivities to chemotherapies and targeted therapies alike. Takundwa said she hopes to partner with researchers in other African countries to expand the use of individualized drug screening.
Sequencing on a Semiconductor
Diseases of blood cells called myeloid cells—including acute myeloid leukemia, myelodysplastic syndromes, and myeloproliferative neoplasms—may look very similar but require different monitoring and treatment strategies. Currently, the gold standard for differentiating between these disorders is genetic sequencing, explained Kojo S.J. Elenitoba-Johnson, MD, chair of the Department of Pathology and Laboratory Medicine at Memorial Sloan Kettering Cancer Center.
Unfortunately, next-generation sequencing is expensive, requires specialized personnel, and can take a significant amount of time. Elenitoba-Johnson and colleagues have developed a semiconductor sequencing platform that measures minute changes in pH that occur when nucleotides are added to a growing DNA or RNA strand—a much cheaper strategy than next-generation sequencing. The Genexus system can process up to eight samples per day, with a same-day turnaround time for results, and the machine can perform basic bioinformatics analysis to aid in the interpretation of data.
The platform accurately identified several single-nucleotide variants, insertions, deletions, and gene fusions in 12 DNA and 12 RNA samples from patients with acute myeloid leukemia, with around 91% concordance with gene alterations found using an existing sequencing platform.
“It’s easy to use, [has a] rapid turnaround time, robust detection of variants from contrived and real-world samples, and it simplifies workflow,” Elenitoba-Johnson said. “It can potentially be used in the future for triaging cases of malignancy.”
Boiling (or Melting) Down Mutational Analysis
Ayman Mohamed, MD, the chief technology officer at Precipio Inc., sought to tackle the same problem as Elenitoba-Johnson using a different technique. Instead of developing a new, sophisticated tool to analyze mutations, Mohamed returned to the basics.
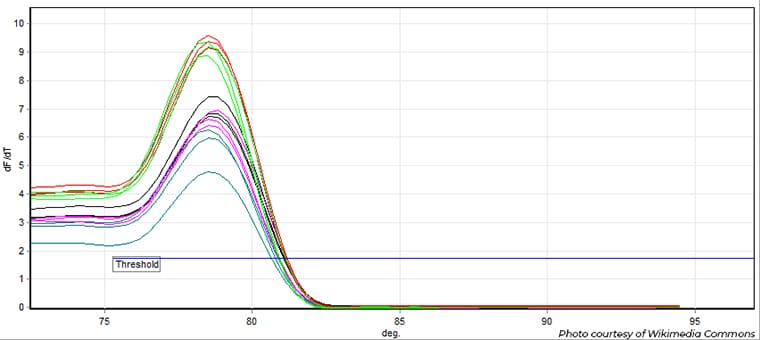
During quantitative PCR analysis, researchers add a probe that fluoresces when it intercalates between DNA strands, allowing for the measurement of the amount of genetic material. The probe can also help determine the melting point of the DNA product—the temperature at which the fluorescent signal disappears, when the probe becomes separated from the DNA.
Because the melting point is closely tied to the DNA sequence, a sample with a different melting point than the wild-type sequence likely harbors a mutation.
Mohamed and colleagues designed a technique called HemeScreen to test whether this approach could identify common blood cancer driver mutations. The platform comes with preplated reagents and controls, along with analysis software, to minimize the expertise needed to conduct the screen. Further, results can be available in a matter of hours.
The researchers compared results from HemeScreen to those from Sanger sequencing and droplet digital PCR in 982 patient samples and saw a near-perfect concordance in its ability to detect mutations in JAK2, MPL, and calreticulin.
“The preplated testing technology enables any simple place that has very limited resources to be able to [adapt to running] major molecular assays … without the need of having this big infrastructure,” Mohamed said.
New Cancer Care Strategies Where They’re Needed
While it’s easy to imagine that designing new technologies is the biggest challenge researchers face when optimizing care in low-resource settings, Dianna Ng, MD, an assistant attending in the Department of Pathology and Laboratory Medicine at Memorial Sloan Kettering Cancer Center, reminded us that integrating these new approaches is an equally formidable process that requires careful consideration.
She touched on the tenets of implementation science—the study of methods to promote the systematic uptake of research findings and other evidence-based practices into routine care. Ng explained that successful implementation requires careful analysis of the problem being addressed, how the new technology will address the problem, how the community will respond to the new technology, and how to measure the outcomes.
Jennifer Dent, president and chief executive officer of BIO Ventures for Global Health, is skillfully employing the tenets of implementation science to boost access to clinical trials in Africa.
Although 18% of the world’s population lives in Africa, only 4% of all clinical trials have included African sites; omitting Egypt and South Africa drops the number to 1%. As cancer researchers around the world strive to understand how genetic ancestry can impact tumor biology and responses to treatment, representation of a globally diverse patient population in clinical research is more crucial than ever, Dent emphasized.
“Patients do best when they are enrolled in a clinical trial. African cancer patients … have not had the same opportunity to be studied in cancer clinical trials, and yet they do have unique tumor biologies, unique genetics,” she said. “It’s really imperative that we expand clinical trials and access to the African continent.”
She and her colleagues launched the African Access Initiative which, in part, aims to boost clinical trial readiness in African hospitals. One project of the initiative—the African Consortium for Cancer Clinical Trials (AC3T)—has comprehensively profiled the diagnostic, treatment, and human resources available at hospitals across seven African countries. These “clinical trial readiness” profiles can help researchers around the world identify African sites that may be amenable to planned trials, and they also demonstrate areas where the AC3T can intervene to help hospitals expand their readiness.
Reducing Costs of Radiotherapy
Radiation is a critical component of treatment for many cancer types, but in many parts of Africa and Southeast Asia, the clinical capacity for radiotherapy is only around a quarter of what it needs to be to meet patient demand, explained Wilfred Ngwa, PhD, an associate professor of radiation oncology and molecular radiation sciences at the Johns Hopkins School of Medicine.
A radiation dosing strategy called hypofractionation delivers a much higher dose of radiation than standard treatment over a significantly lower number of treatments—for instance, five to seven instead of 40, Ngwa said. An extreme version of this, called FLASH radiotherapy, can reduce treatment to a single visit while potentially also decreasing the risk of radiation-induced lung fibrosis. Having fewer appointments lowers the cost and increases the capacity of a treatment center.

But so far, only a handful of tumor types have been shown to benefit from hypofractionated radiotherapy. Researchers are exploring the idea of boosting radiation efficacy by using fiducials—small grains of heavy metal that are injected into the tumors to guide radiation delivery. By loading these metal grains with high-dose immunotherapy, researchers can create a synergistic reaction between the immunotherapy and the naturally immunogenic radiation, at a fraction of the cost of systemic immunotherapy.
Ngwa echoed other presenters’ assertions that collaboration is crucial to implement these strategies into low-resource settings, and that such partnerships can be mutually beneficial. “Right here in the United States, there are also resource-poor settings,” he said. “This is really a win-win opportunity … benefiting the United States and also low- and middle-income countries.”
Cancer Treatment Guidelines at Home and Abroad
With a myriad of therapies approved for each type of cancer, how do oncologists decide how to optimally treat each patient? In the United States, the National Comprehensive Care Network (NCCN)—an alliance of 33 U.S. cancer centers—establishes and revises massive guideline sets for each cancer type to help guide treatment decisions.
“The guidelines are a very important way for both providers and patients to understand what the treatment and diagnostic options are,” said Thomas Flaig, MD, vice chancellor for research and a professor in the Division of Medical Oncology in the School of Medicine at the University of Colorado Anschutz Medical Campus and an NCCN panel member. “It’s putting together evidence in a very logical, consensus manner.”
But how are such decisions made in countries with resource limitations that may affect the practicality of such recommendations?
Flaig discussed the NCCN Framework Guidelines, designed to be adapted to a variety of settings. The framework guidelines address each treatment decision across three levels of infrastructure—basic resources, core resources, and enhanced resources—with treatment guidelines geared toward increasing resource availability.
NCCN is also working closely with the African Cancer Coalition and other organizations to develop a specific set of NCCN Harmonized Guidelines for Sub-Saharan Africa. Through in-depth conversations with leading oncologists representing several African countries, they have published 54 harmonized guidelines to date, featuring annotations for important Africa-specific standards of care and for practices that may be too cost-prohibitive for some providers.
With a membership representing more than 141 countries and territories, the AACR strives to support cancer research and improve patient care in all areas, both domestic and international. For patients living in places where cancer care may be harder to come by, such investments in new technologies, partnerships, and guidelines may make all the difference.


